Brendan Burgess
Founder
- Messages
- 55,384
I just got my Laya renewal .
Flex 500 Explore which I have had for a few years. Great policy. Covers all the hospitals including the hi-tech hospitals. I choose a big excess - €500 per in-patient stay.
I was about to just let it renew automatically, when I decided to check the cover.
I see "Blackrock Clinic and Mater Private: No cover". Surely they should be obliged to highlight any reductions in cover?
I would be raging if I had renewed this automatically and then found I needed the Blackrock Clinic to see that it was no longer covered.
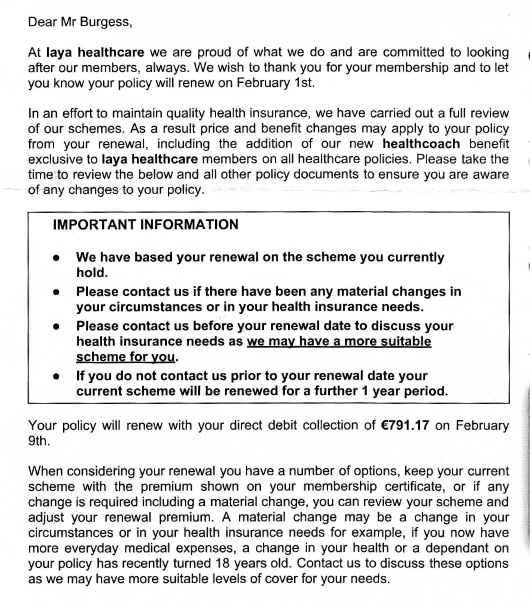
I don't think that the following letter covers it.
Brendan
Flex 500 Explore which I have had for a few years. Great policy. Covers all the hospitals including the hi-tech hospitals. I choose a big excess - €500 per in-patient stay.
I was about to just let it renew automatically, when I decided to check the cover.
I see "Blackrock Clinic and Mater Private: No cover". Surely they should be obliged to highlight any reductions in cover?
I would be raging if I had renewed this automatically and then found I needed the Blackrock Clinic to see that it was no longer covered.
I don't think that the following letter covers it.
Brendan