You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Ireland 2nd out of 19 countries for nurses per capita
- Thread starter Julius
- Start date
NoRegretsCoyote
Registered User
- Messages
- 5,766
Is this based on data from professional organisations or a public body? Or people who tick "nurse" on the Census form? For Ireland I think it's the latter.
I went looking at this years ago and data sources are very different from country to country.
I went looking at this years ago and data sources are very different from country to country.
Childcare is expensive in Ireland. This expense is usually reduced by one partner (usually female) working less hours to concentrate on family issues. In the business, people who work fulltime are known as Whole-Time-Equivalents and anybody working less than fulltime hours is known as a decimal place of that e.g. 0.50 WTE for somebody working half the hours. In my experience of working in three hospitals I've found quite a majority of nurses work less than fulltime hours. Likely, this is an "Irish thing" and the Channel 4 figures might not reflect the true situation for nurses in Ireland.Yep, we have lots of doctors and nurses in Ireland. Getting them to work full time is the problem.
It's an international thing. The data shows that when economic circumstances allow women are more likely to work fewer hours. In other words in you increase their pay they work less. Women tend to work to live, men tend to live to work. We can talk all we like about societal expectations and all that but it it mainly driven by biology, It's just the way we're made.Childcare is expensive in Ireland. This expense is usually reduced by one partner (usually female) working less hours to concentrate on family issues. In the business, people who work fulltime are known as Whole-Time-Equivalents and anybody working less than fulltime hours is known as a decimal place of that e.g. 0.50 WTE for somebody working half the hours. In my experience of working in three hospitals I've found quite a majority of nurses work less than fulltime hours. Likely, this is an "Irish thing" and the Channel 4 figures might not reflect the true situation for nurses in Ireland.
We need to accept that reality and act accordingly. As medicine becomes a more and more female dominated industry we need to train a higher number of doctors to have the same net output of hours.
As we become richer and our State supports become more generous we need to accept that nurses will work fewer hours and train more nurses if we want the same number of net hours worked.
Right Winger
Registered User
- Messages
- 293
Is is indeed an "Irish thing" and it's driven at least partly by our insane tax system that inflicts a top marginal rate on the average industrial wage. Coupled with individualisation, it incentivises second earners to cut back on hours worked and keep their earnings out of the top tax rate.Childcare is expensive in Ireland. This expense is usually reduced by one partner (usually female) working less hours to concentrate on family issues. In the business, people who work fulltime are known as Whole-Time-Equivalents and anybody working less than fulltime hours is known as a decimal place of that e.g. 0.50 WTE for somebody working half the hours. In my experience of working in three hospitals I've found quite a majority of nurses work less than fulltime hours. Likely, this is an "Irish thing" and the Channel 4 figures might not reflect the true situation for nurses in Ireland.
You have to be very careful parsing stats and reports about nursing numbers. Not every country defines a nurse in the same way and some countries leave out some categories. For example, some places will count nurses working in hospitals but not in GP practices or nursing homes. Others will count midwives as part of the whole nursing cohort but others leave them out completely.
When we did a project on this a few years ago we found some studies included healthcare assistants, nursing students, etc. Others included nurse managers, lecturers, even pharmaceutical reps with nursing degrees who were technically registered as nurses but not clinically active. You also have many varying levels of nursing skills, for example the NHS has much higher numbers of specialist nurses and advanced nurse practitioners, roles which don't even exist in some other countries. I haven't seen the Channel 4 report but it is likely missing some of this nuance.
As of 2023, 91% of hospital consultants work full-time (ranging from 87% to 100% depending on specialty). In the UK it is 77%.
Many Irish consultants also work in private hospitals on top of this, in which case you could end up with >100% FTE.
>95% of trainees (whether hospital or GP) work full-time.
GP might seem like a different story as about 84% of GPs in Ireland work full-time. The UK stats are about 75%. In 1992, 97% of GPs in Ireland were full-time. But if you look closer there were fewer GPs per head of population (1:1,800 versus 1:1,600) and they were seeing fewer patients per week on average.
The decline in FTEs in GP may be linked with the increased percentage of women in GP but the changes are not linear, e.g. as female GPs get older they tend to increase their hours. Regardless, the absolute and relative productivity of GPs has increased. We do still need more GPs, but it is largely because of the changing nature of the work rather than the nature of the workers.
I don't know what experience/evidence you are basing this on but I have never once heard a nurse or doctor colleague say they are cutting back their hours for tax reasons. It is virtually always for childcare, looking after older parents, or because of burnout.
When we did a project on this a few years ago we found some studies included healthcare assistants, nursing students, etc. Others included nurse managers, lecturers, even pharmaceutical reps with nursing degrees who were technically registered as nurses but not clinically active. You also have many varying levels of nursing skills, for example the NHS has much higher numbers of specialist nurses and advanced nurse practitioners, roles which don't even exist in some other countries. I haven't seen the Channel 4 report but it is likely missing some of this nuance.
Yep, we have lots of doctors and nurses in Ireland. Getting them to work full time is the problem.
As of 2023, 91% of hospital consultants work full-time (ranging from 87% to 100% depending on specialty). In the UK it is 77%.
Many Irish consultants also work in private hospitals on top of this, in which case you could end up with >100% FTE.
>95% of trainees (whether hospital or GP) work full-time.
GP might seem like a different story as about 84% of GPs in Ireland work full-time. The UK stats are about 75%. In 1992, 97% of GPs in Ireland were full-time. But if you look closer there were fewer GPs per head of population (1:1,800 versus 1:1,600) and they were seeing fewer patients per week on average.
The decline in FTEs in GP may be linked with the increased percentage of women in GP but the changes are not linear, e.g. as female GPs get older they tend to increase their hours. Regardless, the absolute and relative productivity of GPs has increased. We do still need more GPs, but it is largely because of the changing nature of the work rather than the nature of the workers.
There is no evidence for this. It is just like the pseudoscientific propaganda the British Empire promulgated about Irish/Indian/African people being biologically stupid and lazy.We can talk all we like about societal expectations and all that but it it mainly driven by biology, It's just the way we're made.
Is is indeed an "Irish thing" and it's driven at least partly by our insane tax system that inflicts a top marginal rate on the average industrial wage. Coupled with individualisation, it incentivises second earners to cut back on hours worked and keep their earnings out of the top tax rate.
I don't know what experience/evidence you are basing this on but I have never once heard a nurse or doctor colleague say they are cutting back their hours for tax reasons. It is virtually always for childcare, looking after older parents, or because of burnout.
Why be amazed by stuff on Channel 4, after all, don't they broadcast other quality programmes like "Celebrity Detox" and other factual offerings?Report on Channel 4 tonight about a study in UK that shows UK in 15th place out of 19 western countries for nurses per capita. I was amazed to see that Ireland was 2nd.
Lies, damned lies, and statistics from unknown sources and compilers.
Can you post a link for that please? The only information I can find on that is a survey of GP's who were asked about their work practices. In the UK only one in four GP's work fulltime (37.5 hours a week or more). I find it hard to believe that three times as many work full time here.You have to be very careful parsing stats and reports about nursing numbers. Not every country defines a nurse in the same way and some countries leave out some categories. For example, some places will count nurses working in hospitals but not in GP practices or nursing homes. Others will count midwives as part of the whole nursing cohort but others leave them out completely.
When we did a project on this a few years ago we found some studies included healthcare assistants, nursing students, etc. Others included nurse managers, lecturers, even pharmaceutical reps with nursing degrees who were technically registered as nurses but not clinically active. You also have many varying levels of nursing skills, for example the NHS has much higher numbers of specialist nurses and advanced nurse practitioners, roles which don't even exist in some other countries. I haven't seen the Channel 4 report but it is likely missing some of this nuance.
GP might seem like a different story as about 84% of GPs in Ireland work full-time.
There's no "if" about it. This study from the NHS shows that 42% of female doctors worked less than full time. That figure was only 7% for male doctors. That is almost totally linked to having children.The decline in FTEs in GP may be linked with the increased percentage of women in GP but the changes are not linear, e.g. as female GPs get older they tend to increase their hours. Regardless, the absolute and relative productivity of GPs has increased. We do still need more GPs, but it is largely because of the changing nature of the work rather than the nature of the workers.
What, that women and men behave differently in work? I don't think that's pseudoscience promulgated by the British Empire.There is no evidence for this. It is just like the pseudoscientific propaganda the British Empire promulgated about Irish/Indian/African people being biologically stupid and lazy.
Yes, they want to work less to send time with their children and when economic circumstances allow they do so. Therefore a pay increase is what allows that to happen. There's an American study on it but I can't find it at the moment.I don't know what experience/evidence you are basing this on but I have never once heard a nurse or doctor colleague say they are cutting back their hours for tax reasons. It is virtually always for childcare, looking after older parents, or because of burnout.
@arbitron above makes some good points, Even nurses who worked in Italy's health service do not have all their qualifications recognised in Ireland and must sit exams before they can work as nurses here. Furthermore, many nurses in other countries do the work Health Care Assistants do in Ireland. These points throw some dark on Channel 4's figures.
Which is nonsensical and a barrier to entry.@arbitron above makes some good points, Even nurses who worked in Italy's health service do not have all their qualifications recognised in Ireland and must sit exams before they can work as nurses here.
That means our figures for nurses are understated.Furthermore, many nurses in other countries do the work Health Care Assistants do in Ireland.
I'd love to see the role of Nurse Practitioner become common here. They can do many of the things that doctors do.
I agree that it's very hard to do a like for like comparison.These points throw some dark on Channel 4's figures.
With roughly 11,000 hospital doctors (consultant and NCHD) in Ireland versus 4,300 GPs, hospital doctors make up 72% of all doctors.
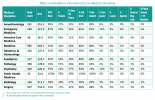
This table summarises the hospital consultant numbers.
Public health is 78% female but 100% of them work full time. Emergency medicine is 31% female but "only" 85% work full time. I don't see any link between feminisation and decreased WTE.
The WTEs there do not include the non-clinical management work that many Consultants do, e.g. medical director of a hospital, so the "89% full-time" headline rate is an underestimate of the total work product.
OECD 2023 figures for part-time employment across the Irish workforce is 19.6%. Consultants are at half of that and NCHDs/trainees even lower. Hospital doctors are already at a higher WTE rate than most workers so it's just not true that "Getting them to work full time is the problem."
If we look at GPs alone, then the latest figures for full-time practice are 75% to 84%, depending on the source. Let's be pessimistic and take the lower figure of 75%. That means about 1,100 GPs are working less than full time. But they are not working zero hours. They may be doing 4 days, 3 days, etc. Let's be drastic and say they are all doing 2.5 days a week. So that means about 550 fewer GP WTEs.
Therefore out of 15,000+ doctors (hospital & GP), if we take the most negative approximation, we have maybe 1,600 WTEs fewer due to part-time work.
References:
This table summarises the hospital consultant numbers.
Public health is 78% female but 100% of them work full time. Emergency medicine is 31% female but "only" 85% work full time. I don't see any link between feminisation and decreased WTE.
The WTEs there do not include the non-clinical management work that many Consultants do, e.g. medical director of a hospital, so the "89% full-time" headline rate is an underestimate of the total work product.
OECD 2023 figures for part-time employment across the Irish workforce is 19.6%. Consultants are at half of that and NCHDs/trainees even lower. Hospital doctors are already at a higher WTE rate than most workers so it's just not true that "Getting them to work full time is the problem."
If we look at GPs alone, then the latest figures for full-time practice are 75% to 84%, depending on the source. Let's be pessimistic and take the lower figure of 75%. That means about 1,100 GPs are working less than full time. But they are not working zero hours. They may be doing 4 days, 3 days, etc. Let's be drastic and say they are all doing 2.5 days a week. So that means about 550 fewer GP WTEs.
Therefore out of 15,000+ doctors (hospital & GP), if we take the most negative approximation, we have maybe 1,600 WTEs fewer due to part-time work.
References:
- Medical Workforce Report 2022-2023 (HSE - National Doctors Training & Planning)
- Structure of General Practice in Ireland 1982 — 2015
- Future career intentions of recent GP graduates in Ireland: a trend analysis study
- How many general practice consultations occur in Ireland annually? Cross-sectional data from a survey of general practices
- OECD (2023) Part-time Employment Rate Indicator
I agree with you that ANPs/AMPs are brilliant to work with and make a big difference to a team, but it's by no means a panacea and management are often cagey.I'd love to see the role of Nurse Practitioner become common here. They can do many of the things that doctors do.
It takes a minimum of 8 years from leaving cert to first day as a qualified ANP/AMP and the salary begins at €65k.
8 years after the leaving cert a doctor will be starting as a 3rd year SHO on €51k or even a junior reg on €59k but with a much broader scope of practice than an ANP, i.e. can legally do more for less pay.
We tried to get an ANP for our service and the hospital basically said why would we do that when we can pay a junior doctor less money to do more? Junior doctors also rotate on 6-month or 12-month contracts, much easier to manage if not performing.
@arbitron, I've worked as a quality manager and my current role includes process and systems design to increase efficiency. It is almost always the case that organisations and processes that have evolved organically are inefficient. In my limited experiences of Hospitals they seem grossly inefficient with massive duplication of process, inefficient data collection and transfer, almost no patient tracking and no real time monitoring of patient flows. Therefore when I hear about staff shortages and lack of resources my first reaction is that the problem is misallocation of resources and inefficient processes that waste the time of valuable and scarce human resources. We have plenty of nurses and doctors and we've had one of the best funded healthcare systems in the world for the last 3 decades. We just structure and run it very badly.
And yet as of 2022 the Medical Council have 21,680 registered with 18,424 who are clinically active. That number is increasing year on year.Therefore out of 15,000+ doctors (hospital & GP), if we take the most negative approximation, we have maybe 1,600 WTEs fewer due to part-time work.
Then there's the fact that many doctors working in General Practice are not GP's. Only the principal Doctor has to be vocationally trained. It's the other doctors, which make up over one third of those on the Medical Register and are categorised as "General", the ones that are working for the GP, that I'm talking about. I can't find any solid data for them.
While we have 3.5 doctors per 1000 people, which puts us ahead of the UK, France and USA, but behind Spain and Portugal, it doesn't really tell us anything. The same is true for the figures on Nurses.
Edit: In 2020 there were 4899 doctors on the Medical Register who self declared as working in General Practice. The average consultation time per visit is 13.7 minutes. There were 21,353,731 GP consultations. Therefore the average amount of time that a doctor working in General Practice spent seeing patients, based on a 48 week working year, is 20.73 hours a week. If they spend 50% more time on top of that doing non-patient facing work then the average doctor working in General Practice works between 31 and 32 hours a week. Source This data is not accurate but it is indicative.
Vocationally trained GP say that they work an average of over 50 hours a week, That means a large cohort of doctors working in general practice work part time.
Last edited:
@arbitron, I've worked as a quality manager and my current role includes process and systems design to increase efficiency. It is almost always the case that organisations and processes that have evolved organically are inefficient. In my limited experiences of Hospitals they seem grossly inefficient with massive duplication of process, inefficient data collection and transfer, almost no patient tracking and no real time monitoring of patient flows. Therefore when I hear about staff shortages and lack of resources my first reaction is that the problem is misallocation of resources and inefficient processes that waste the time of valuable and scarce human resources. We have plenty of nurses and doctors and we've had one of the best funded healthcare systems in the world for the last 3 decades. We just structure and run it very badly.
I couldn't agree with you more. We have plenty of people, we just don't use them very well and we don't give them the right tools and environments to work at the top of their training. That's different from saying we need them to work more hours though, which was the original point made.
Has any body, an individual or an organization, measured outcomes for the "medical industry"? Efficiency measures costs for the same activities irrespective of outcomes. Effectiveness turns the equations on their heads and measures the product of all this activity across all disciplines and professions, nursing, medical, physiotherapy, etc, and identifies how many patients were treated, how many were "cured", returned to good health, either in the home or outside it or both, how many avoided death or severe disability?
The reason for all these frenetic measuring jags people get involved in is quite frankly irrelevant unless and until effectiveness is measured. It seems the only measure that matters is cost (efficiency). Why not focus on outcomes (effectiveness) for a change?
The reason for all these frenetic measuring jags people get involved in is quite frankly irrelevant unless and until effectiveness is measured. It seems the only measure that matters is cost (efficiency). Why not focus on outcomes (effectiveness) for a change?
Right Winger
Registered User
- Messages
- 293
@mathepac That's not really enough. Sure, effectiveness is the ultimate aim and, without it, all the efficiency in the world is pointless. But in a real world scenario, resources are limited, and therefore the quantity of output you achieve (aka effectiveness) will increase with increased efficiency. So you need both.
The other major problem with focussing on effectiveness, and ignoring efficiency, is that it is a licence for featherbedding and nest building by insiders. Services are run for the benefit of the providers rather than the public. Lest there be any doubt about that, the ongoing relevations in RTE amply demonstrate the pitfalls.
The other major problem with focussing on effectiveness, and ignoring efficiency, is that it is a licence for featherbedding and nest building by insiders. Services are run for the benefit of the providers rather than the public. Lest there be any doubt about that, the ongoing relevations in RTE amply demonstrate the pitfalls.
"Quantity of output" is an efficiency measure, not an effectiveness measure, IMO as you're attempting to do more for the same or lower cost without measuring outcomes.But in a real world scenario, resources are limited, and therefore the quantity of output you achieve (aka effectiveness)
There will usually be a number of factors which influence the decision to work part time. Very high marginal tax rates combined with very high childcare costs combine to make it economically unattractive for parents with young children to both work full time. Given that women are far more likely to want to be the one to spend more time with young children, for obvious biological/evolutionary reasons, as women come to dominate Medicine in general (around 60% of Irish graduates are women) and general practice in particular finding ways to keep them working as much as possible makes good economic sense. That's a different issue to the inefficiency that's baked into the entire industry and it's not the same as "making them work more hours" but workforce participation rates should be part of the discussion when you are discussing a workforce.I couldn't agree with you more. We have plenty of people, we just don't use them very well and we don't give them the right tools and environments to work at the top of their training. That's different from saying we need them to work more hours though, which was the original point made.