Brendan Burgess
Founder
- Messages
- 55,613
From the HIA website
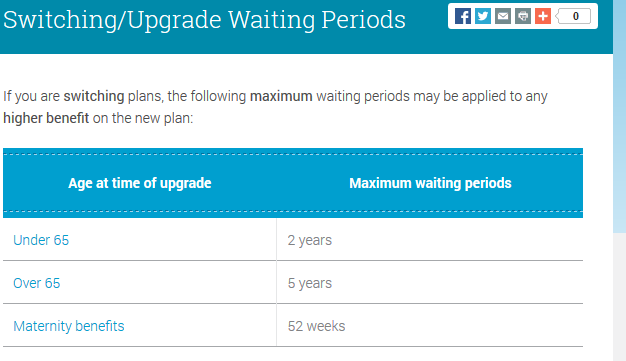
If I have a basic plan with Laya and upgrade to a bells and whistles plan, I have to wait for 2 years for the extra cover for existing illnesses.
But what if I switch from Laya to Aviva? How can they say whether I have extra cover or not? For example, I have a €500 excess on my current Laya policy. If I get similar cover without the excess from Aviva, do I have to wait 5 years?
Policies are difficult to compare, so I can't see how they can answer this question.
If I have a basic plan with Laya and upgrade to a bells and whistles plan, I have to wait for 2 years for the extra cover for existing illnesses.
But what if I switch from Laya to Aviva? How can they say whether I have extra cover or not? For example, I have a €500 excess on my current Laya policy. If I get similar cover without the excess from Aviva, do I have to wait 5 years?
Policies are difficult to compare, so I can't see how they can answer this question.
Last edited: